A child getting burned is a nightmare scenario for any parent or caregiver. Burns in children are most commonly scalding accidents (80%) involving hot water or steam, or open flame burns (14%).
Burns lead to trauma and disability, and can result in a long hospital stay, multiple surgeries and sometimes, life-long impairment of functions. Generally, the more severe the burn, the more likely your child is to need hospital admission, critical or intensive care, and surgery.
First steps: Assessment of burn severity
First aid involves making the child safe (e.g. remove them from the hazard, extinguish the flame etc) and arresting the burn process. This is done by cooling. Remove clothes involved in the scald or burn, irrigate the area with cool water. Cooling cloths, cooling gels as you take the child to the medical centre will help.
Your treatment team will need to decide whether the burn is a “see and treat” or a “see and send”.
This decision is based on burn severity. These grades are assessed based on several factors:
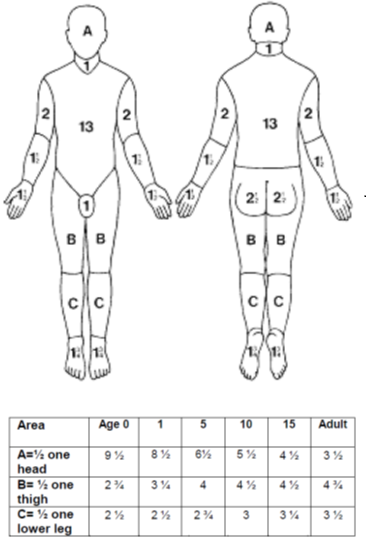
1.Size of burn area: There are several ways to assess area burned. Generally, the team will map the burned areas and assign a percentage e.g. 15% burns.
2. Depth of burn: You may have heard of 1st, 2nd and 3rd degree burns.
3. Body areas
4. Mechanism
A 1st degree burn is superficial and affects the top skin layers. It is quite painful and may increase redness in that area, but the skin remains unbroken in most parts. Scalding injuries and sunburn are good examples.
2nd degree burns involve deeper layers of the skin. The skin is broken , blistering and weeping in parts. These are painful too, as the nerves within the deeper skin layers are triggered. Contact injuries e.g. hot iron, can create burns like this.
3rd degree burns are deeper still. All the skin layers are burned, leaving connective tissue overlying the fat and muscles (fascia) exposed. These take on a dry, waxy, leathery appearance. These are severe because these deeper structures tissues will need to be covered , and skin may need to be taken from other body areas (grafted) to achieve this.
Special body areas:
Burn site matters. Burns to certain body areas are considered severe, due to the level of disability or disfigurement resulting. These special areas are:
1. Face
3. Airway/ inhalation injuries: a burn that affects the throat externally or internally can lead to breathing problems
2. Genitals and perineum
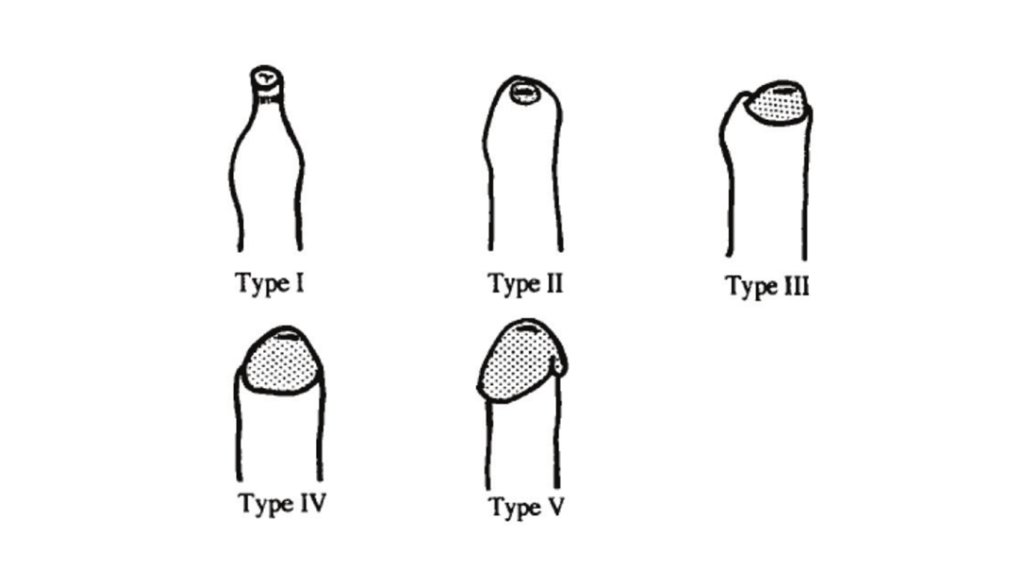
4. Hands and feet
Special mechanisms
Some mechanisms of injury can cause more damage than others. For example:
-Electric burns have an unpredictable course, causing damage between the current’s entry site and its final discharge site
-Chemical burns may need specialised treatment with neutralising agents
If in doubt, treatment teams can seek specialist input from a hospital specialised to deal with burns.
The burn is severe. Now what?
Small and superficial burns can be treated with first aid. Treatment teams will make a plan for pain control, and monitoring the burn area to ensure there is no infection developing. However, the body heals by forming scars. Therefore, burns in sensitive areas e.g. hands will need a plan for follow-up, to ensure that scarring does not lead to disability.
More severe burns need immediate stabilisation. The child will receive a cannula and a drip will be started. Keeping the child hydrated is part of immediate resuscitation.
If there is significant concern about fluid loss, a catheter tube may be used to empty the bladder and measure urine volume produced.
If there is concern about the throat closing over due to smoke inhalation or face and neck burns, a breathing tube may be placed to secure the airway and enable breathing.
Bigger, deeper burns, or burns involving special body sites need specialist review i.e. “see and send”.
Different countries and regions have diverse ways of organising burns services. However, the priority for treatment is:
Early
–effective pain control
-prevent dehydration from fluid loss
-prevent infection, leading to sepsis
During this phase of injury, severe cases may require treatment in intensive care, to support breathing , circulation and sepsis prevention and treatment. General and plastic surgeons may be involved , to begin the management of wounds and supported healing.
Mid term to late
-prevent scarring
-prevent loss of function / disability
For this phase of injury, the child may need input from general and plastic surgeons with specialist knowledge in this area.
Importantly, the psychological consequences of injury should be considered and support put in place.
Non-accidental injury
As part of a child’s safety, treatment teams will think about non-accidental injury. Treatment teams must consider the mechanism of injury, and how it may be prevented from happening again. This will involve a review of the child’s medical, social and education history. Parents and care givers may be asked probing questions. Ultimately, the goal is to prevent further episodes and ensure the child’s and family’s safety.
Global trends
In 2018 the World health organisation launched the Global Burn Registry. From these data, it appears that burns occur most commonly in children from middle-income countries. In 2021, review of these data demonstrated and average age of 5 years, and that 60% were boys.